Digesting It All!
The digestive system, or gastrointestinal (GI) tract, is a very complex machine requiring many different organs to work together in concert. The ultimate job of the GI tract is to absorb or admit the nutrients necessary to keep the body healthy, while at the same time rejecting or dispelling those substances that are toxic. To accomplish this important job, the membrane that lines the entire GI tract acts as a selective barrier—essentially taking in what is “good” and rejecting that which is “bad.”
There are three key steps to the digestive process: absorption, assimilation and elimination. Absorption begins the moment food crosses from the outside world into the long intestinal tube that makes up the GI tract. As food makes its way through the intestines, absorption continues across the intestinal wall and into the bloodstream. Assimilation is the step whereby nutrients actually enter the cells of the body; and finally,elimination may be thought of as the clean-up process, whereby the body gets rid of the waste products.
Not surprisingly, these critical steps require an incredible amount of energy to get the job done. A very large blood supply is also necessary and, in fact, the GI tract has the largest blood supply of any system in the body. It uses one-third of the overall blood flow from the heart to carry out its continual work.
Normal Flora of the GI Tract
What are the factors involved in healthy digestion? One key component is the internal “ecosystem” of the digestive tract. This self-contained environment within the walls of the stomach, colon, and intestine is the home of more than 400 species of bacteria—most of which are beneficial and protective in their roles. These normal or “friendly” flora of the GI tract number in the trillions, the majority of which reside in the colon. In fact, healthy adults typically have five to eight pounds of living bacteria in their GI tract.
The reason we have so much bacteria happily living in our digestive system is that they produce nutrients essential to digestion. These bacteria actually nourish the cells of the GI tract by producing essential short-chain fatty acids. Moreover, a number of other important nutrients are produced only through the bacterial fermentation of our food. Without the nutrients from this friendly flora, the lining of the GI tract would not function properly.
Another normal and healthy component of the digestive system is a strain of yeast called Candida Albicans, or candida for short. Candida is ubiquitous, covering virtually every living thing on this planet. Under healthy conditions, it does not cause health problems, but when the delicate balance that normally exists inside the body is tipped, candida can grow out of control and create a wide array of mild to severe health disorders. This then becomes a candida infection or candidiasis.
Tipping the Balance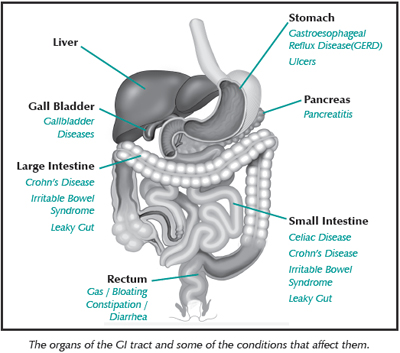
If dangerous bacteria, parasites, or an overgrowth of candida replace the friendly bacteria that line the GI tract, a process of inflammation can begin. This process may even affect other cells and organs of the body that are susceptible to inflammation.
According to Dr. Joseph McWherter in Avoiding Breast Cancer, candida produces estrogen-like compounds that can disrupt normal hormonal function. For example, an over-growth of candida can lead to excessive estrogen production. When candida grows out of control, it can also release part of its fungal wall, which induces inflammation. Such chronic inflammatory changes may eventually disrupt the surrounding environment of the breast cell. Adverse changes to the normal intestinal bacterial flora, such as that caused by long-term use of antibiotics, can double the risk of breast cancer.
An overgrowth of yeast in the intestines can lead to a wide variety of chronic digestive problems, such as bloating, diarrhea, chronic stomach inflammation, and heartburn. It can also cause symptoms that include fatigue, headaches, muscle aches, and chronic flu-like symptoms. Beyond these digestive and systemic discomforts, candidiasis is also often associated with female disorders like chronic vaginal discharge, chronic vaginal yeast infections, chronic urinary canal inflammation, vaginitis, premenstrual syndrome, endometriosis, painful breasts, and other hormonal imbalances.
Common Symptoms of GI Disorders
The symptoms of many of the major digestive system disorders are not specific to just one disease or condition. Abdominal pain, diarrhea, gas, bloating, and constipation can accompany any of the GI health issues, so it may be helpful to review these uncomfortable symptoms.
Abdominal pain can vary in its location, frequency, and intensity with any kind of GI disorder. What is important to know is that certain kinds of abdominal pain, such as that described for pancreatitis, may signal a serious problem.
Diarrhea is the frequent passage of watery stools and is most often caused by intestinal irritation, incomplete digestion of food, use of certain drugs, food poisoning, or food allergies.
Gas and/or bloating occurs when there is excessive gas in the stomach and intestines (also called flatulence) and can be a sign of incomplete digestion. Three major sources of gas in the GI tract are gas swallowed from the air, a gas formed by a chemical reaction of hydrochloric acid from the stomach and pancreatic secretions, and gases formed through bacterial fermentation in the colon. Those who are lactose intolerant or overly sensitive to foods such as legumes and cruciferous vegetables may experience increased gas production.
Constipation refers to infrequent or incomplete bowel movements, often characterized by stools that are hard and difficult to pass due to slow transit time through the GI tract. Usually this is caused by insufficient dietary fiber, excessive dietary fat and or refined foods, side-effects of some medications, lack of exercise, dehydration or hormonal changes.
Digestive Diseases or Conditions
Irritable Bowel Syndrome
Irritable bowel syndrome (IBS) is a catch-all term for a multitude of symptoms and conditions that may involve any part of the GI tract, including the esophagus, stomach, small intestine, gallbladder, colon and bowel. Other commonly used terms that fall into this category include colitis, spastic colon or spastic colitis.
With IBS, the normally rhythmic muscular contractions of the GI tract become uncoordinated and irregular, which interferes with the normal movement of food and waste, often leading to accumulation and potentially a partial obstruction. Symptoms are similar to those of many GI disorders: pain, diarrhea, loss of appetite, nausea and vomiting.
Inflammatory Bowel Disease (Crohn’s Disease and Ulcerative Colitis)
Inflammatory bowel disease (IBD) is another catch-all term for chronic inflammation in the intestines. Crohn’s Disease and Ulcerative Colitis are two forms of IBD, both of which are potentially serious and can lead to malnutrition. In Crohn’s Disease, ulcerations occur along the small or large intestines, and the bowel wall thickens causing the GI tract to narrow, with all layers of affected tissue going through cycles of inflammation, damage and healing. The most common symptom is diarrhea. Ulcerative Colitis is a chronic inflammation of the large intestine. Symptoms include abdominal pain, diarrhea and rectal bleeding. Both diseases can cycle through periods of remission and flare-ups
Celiac Disease
In those with a genetic predisposition, this inflammatory disorder of the small intestine is triggered by exposure to gluten (wheat protein). This condition results in a malabsorption of nutrients; those affected may develop anemia due to a lack of iron, folate, and/or vitamin B12; or osteoporosis due to inadequate absorption of calcium and vitamin D. Celiac disease can lead to fertility problems in women if left untreated. Gas, abdominal cramping, weight loss, canker sores, fatigue and anemia all suggest difficulty digesting gluten and are common symptoms.
Gallbladder Disease
Gallbladder problems typically stem from inflammation, swollen ducts that restrict bile flow,or gallstones that block bile flow. A sedentary lifestyle, being overweight, and skipping meals are common factors in those with gallbladder problems. Food allergies can also trigger inflammation. Symptoms include indigestion, chronic gas, bloating, fatigue, and anxiety in chronic cases; and severe pain, nausea, and vomiting in an acute gallbladder attack.
Gastritis
Gastritis is an inflammation of the lining of the stomach that involves erosion of the upper-most mucosal layer. While many types of gastritis cause no symptoms, those that do can result in heartburn, pain in the upper abdomen, nausea, and vomiting.
Gastroesophageal Reflux Disease (GERD)
Often referred to as heartburn, this condition occurs when partially digested food from the stomach, along with hydrochloric acid (HCl) and enzymes, backs up into the esophagus (a process also known as reflux). The acidity of HCl may damage the delicate lining of the esophagus. Reflux (or regurgitation), chest pain, and difficulty swallowing are some of the most common symptoms of GERD.
GI Tract Infections
Although parasites, bacteria, viruses, fungi, worms, and protozoa are ubiquitous, some can wreak havoc when infecting the GI tract. Some organisms can provoke hormone changes by binding estrogen, thus making it unavailable, while others can actually produce hormones leading to excess levels. Infections can cause a wide range of symptoms including diarrhea, cramps, gas, and fatigue.
Leaky Gut Syndrome
The leaking of the gut wall through gut lining can be triggered by a number of factors including food allergies, alcoholism, radiation, chemotherapy, infections and severe trauma. This compromises the barrier function of the digestive tract so that toxins and bacteria can seep into the bloodstream and be passed along to the liver. While common symptoms include vitamin deficiencies, gas, cramping, fatigue, and poor concentration, the development of an autoimmune disease (including allergies) may also be a sign of leaky gut syndrome.
Pancreatitis
Inflammation of the pancreas usually results from the blockage of the ducts of the pancreas and can be caused by alcohol abuse, viral infection, or when gallstones become trapped in the ducts. The most classic symptom of acute pancreatitis is pain above the navel that spreads across the abdomen and to the back. Other symptoms may include nausea, vomiting, fever, and weakness.
Ulcers
Ulcers are sores or lesions that develop in the mucus lining of the stomach. Once believed that stress was the major cause of peptic ulcers, most are associated with the presence of a bacterium called Helicobacter pylori between the lining of the stomach and the protective mucous layer. Common symptoms include severe pain (often worse between meals and at night) and black, tarry stools, which indicate internal bleeding.
Hormones and the GI Tract
Oral Progesterone Supplementation
A study conducted by Dr. Joel Hargrove et al. found that the absorption of oral progesterone is indeed influenced by certain factors. These factors include the micronization of progesterone particles in the normal absorption of fats in the GI tract. In particular, they showed that by mixing micronized progesterone with an edible oil in a capsule, progesterone was more easily absorbed by the GI tract and transported to the bloodstream, making it more available to the body.
Adrenal Hormones
According to a 2012 study, both DHEA and cortisol levels “may be involved in exacerbating abdominal symptoms in individuals with IBS.” Study participants, some of whom were previously diagnosed with IBS, were exposed to stressful conditions and tested for hormone levels before, during, and after the stressful event. The subjects with IBS had lower circulating DHEA levels and a higher ratio of cortisol to DHEA than subjects without IBS.
These results are not surprising because the adrenal hormones are key players in the immune system. DHEA, in particular, can affect healing from a GI tract disorder. In the case of intestinal tract allergies or invasion by pathogens, major inflammation may occur. DHEA, which promotes cell growth and repair, can help speed up the repair of the inflamed mucosal tissues in the GI tract.
Cortisol, while typically associated with stress, also plays a role in the repair and healing of GI tract disorders. Cortisone, a synthesized form of cortisol, acts as an anti-inflammatory and anti-viral agent and is often prescribed for people suffering from IBS.
Female Hormones
The hormones we think of as female hormones (primarily estrogen and progesterone) also have significant effects on the health of the GI tract. The imbalances of these hormones can influence the movement of food through the intestines—some by speeding the process up, causing diarrhea, nausea, and abdominal pain; and others by slowing things down and causing bloating and constipation.
It is quite common for post-menopausal women to be constipated. One study set out to test the effects of the female sex hormones progesterone and estradiol on the bowel movements of healthy postmenopausal women. The results showed that supplemental progesterone actually decreased the time it took for the colon to empty. The combination of progesterone and estradiol also produced looser stools and relief from constipation.
Women often notice changes and experience other GI tract discomforts (diarrhea and bloating, for example) throughout their menstrual cycle. These symptoms are most common during the luteal phase or second half of the cycle. The increased production of progesterone and estrogen during a woman’s menstrual cycle may have a direct effect on the digestive system. Such hormonal fluctuations may cause changes in the natural ecosystem of the GI tract and indirectly lead to GI tract discomfort. In The Yeast Syndrome, Dr. John Trowbridge notes that candida growth flares with increases of progesterone.
The gallbladder stores bile, which is released when we eat fatty foods, in order to aid in the digestion and absorption of fats. When hormone balance is disturbed so that it favors estrogen excess, or supplemental estrogens are taken in the form of Premarin or birth control pills, bile tends to thicken and may ultimately lead to the development of gallstones.
The digestive system plays an important role in the proper disposal of estrogen from the body. When the bowel does not function properly, estrogen that is meant to be excreted by the intestines is sometimes recycled and reabsorbed into the bloodstream.
Excess activity of a specialized enzyme called beta-glucuronidase, which is involved in the reactivation of estrogen and prevents it from leaving the body, may also be responsible for the recycling and build-up of estrogen levels. The excess activity of beta-glucuronidase is triggered by an imbalance of the normal ecosystem of the GI tract.
Natural progesterone can be beneficial with regard to the gut’s healing process, according to Dr. Paul Lynn in the book Optimal Digestive Health. He frequently recommends progesterone for women with digestive disorders, and as a hormone with both anti-inflammatory and anti-stress properties, it has been shown to work as a natural relaxant in the GI tract.
Other Hormones at Work in the Gut
Thyroid hormone levels can also affect the proper functioning of the digestive system. In cases of hypothyroidism (when thyroid levels are too low), digestion in the stomach and intestines slows down, and the concentration of stomach acid and digestive enzymes may be diminished. Chronic constipation is a recognized symptom of hypothyroidism.
Finally, melatonin (a hormone produced primarily in the brain) also seems to alleviate the painful and bothersome symptoms of IBS. While melatonin from the brain is critical to sleeping and waking cycles, some melatonin is also produced in the stomach when we eat. This form of melatonin regulates the production of stomach acid and the enzyme pepsin, as well as the movement of food from the stomach. In one study, patients who took melatonin daily showed decreased gastrointestinal pain and rectal pain, and more frequent bowel movements.
Conclusion
Given the many organs that comprise the digestive system and its complex internal environment—home to hundreds of species of normally friendly bacteria—it should not come as a surprise that the GI tract is susceptible to a wide range of disorders.
To keep the GI tract functioning properly, there are many factors to consider. From the foods we eat to the general ways in which we practice good health (such as adequate sleep and exercise), these factors can all influence the digestive system. And, as discussed here, hormone levels are another important factor.
While not intended to be comprehensive, we have introduced you to some of the roles that estrogens, progesterone, DHEA, cortisol, thyroid, and melatonin hormones play in the absorption, assimilation, and elimination functions of the GI system. It is important to consider the role of hormone balance and “digest” all that is presently known when it comes to keeping your digestive system as healthy as possible.
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding any condition or medication. Do not disregard professional medical advice or delay in seeking it because of something you have read on this site.

